

The cardiologist inserts a catheter (a thin plastic tube) into the large vein, threading it up to the heart.

Catheterization: This minimally invasive approach involves only a small needle puncture in the leg.This approach may be necessary in babies who are especially small, or who have other congenital heart defects that require treatment. Surgery: Using a traditional surgical approach, the surgeon makes an incision between the ribs on the left side of the baby’s chest, using either sutures or a clip to close the ductus.If medication isn’t effective or a baby’s health is endangered, catheterization or a surgical procedure may be required to close the PDA. Medication may be prescribed to help the ductus close. In many cases a PDA will resolve on its own in the first few months or at least within the first year of life. Over time, the additional blood flow to the lungs can put adults at risk for such serious problems as pulmonary hypertension and heart rhythm abnormalities. In rare cases, PDAs aren’t diagnosed until adulthood. This makes feeding difficult and also raises risk of abnormal neurodevelopment. If this happens, a baby may need mechanical ventilation for a long period of time. Larger PDAs can cause extra blood to flow into the lungs, which can increase pressure in the lung arteries, putting a strain on the heart, and even cause heart failure. Some small PDAs may cause no symptoms at all and will close on their own before the child is a year old. It then becomes a burden on the circulation, as opposed to supporting circulation,” Dr. “If a baby is born prematurely, then the signals for the ductus arteriosus to close often don't work very well, and the ductus might stay open. This is necessary for the proper development of circulation. In a fetus, the ductus arteriosus allows blood to be pumped directly from the heart to the aorta, the main artery of the body, without going through the lungs. However, only recently have techniques and devices been developed to address this problem in small, prematurely born babies. Catheterization techniques to close a PDA were developed in 1990s and are now the standard of care in children. Though the procedure is life-saving, it can be traumatic for a small body. The traditional treatment for a PDA that doesn’t close naturally is heart surgery. “PDA leaves a hole that might be three to five millimeters in diameter-so pretty small, but in a small baby that can be a big problem,” says interventional cardiologist Jeremy Asnes, MD, chief of pediatric cardiology for Yale Medicine and co-director of the Yale New Haven Children’s Hospital Heart Center. If this doesn’t happen, the baby has PDA, a condition that may require intervention. Once a baby is born and begins breathing through its own lungs, the ductus arteriosus begins to narrow and is meant to close within a few days. (The word “patent” means “open” in Latin.) The ductus arteriosus is a temporary blood vessel that, in fetuses, allows the blood to skip circulation to the lungs, because oxygen is delivered through the mother’s placenta.
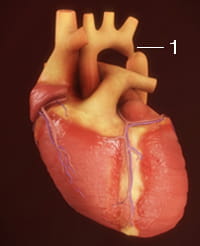
Patent ductus arteriosus (PDA) is a congenital heart defect that is common in babies born prematurely, but rare when pregnancies go full-term.


 0 kommentar(er)
0 kommentar(er)
